| Latest Forum Topics / Biosensors |
|
|
Is Biosensors a good buy?
|
|||||
|
bengster68
Master |
25-Jun-2008 23:20
|
||||
|
x 0
x 0 Alert Admin |
Study Might Ease Stent FearsBy JON KAMP
June 25, 2008; Page D2 Patients with clogged arteries treated after the first drug-coated stent reached the U.S. market this decade were less likely to need repeat procedures and weren't more likely to die or have a heart attack, according to a study released Tuesday.
The study, set for publication in the Journal of the American Medical Association, may further ease concerns about stent safety. It was assembled from claims data on about 67,000 Medicare patients who were treated before and after the first coated stent, from Johnson & Johnson, was approved in early 2003. The now-$4 billion global market for coated stents has been damaged by concerns that first-generation devices elevate the risk for dangerous clots, but those worries appear to be fading because of more favorable studies. The new study has limitations because it isn't a randomized trial with a direct product-to-product comparison, and it may reflect doctors' biases in choosing devices for certain cases. Also, while only one coated stent was available during the study period, the marketplace is more crowded now. But the study covers a very large population that clearly saw coated-stent benefits that outweighed the risks, said David Malenka, a cardiologist at Dartmouth-Hitchcock Medical Center in Lebanon, N.H., and the study's lead author. This has been a big question ever since safety concerns became inflamed in 2006. "Everything boils down to understanding risks and benefits," Dr. Malenka said. "I think this helps put it into perspective." The new study was supported by the National Institute on Aging and the Robert Wood Johnson Foundation, which was founded by the family that started Johnson & Johnson. A spokesman for J&J's stent-making Cordis subsidiary said the company wasn't involved in funding the study. Dr. Malenka has received research funding from Abbott Laboratories and Guidant Corp.'s endovascular business, which is now part of Abbott. While this study only includes a coated stent that is expected to see decreased use as competition increases in the U.S., perhaps muting its impact, Dr. Malenka said he feels the results have broader application. A view that includes newer coated stents would likely show a greater benefit, he suggested. J&J was first to the U.S. market, and Boston Scientific Corp. joined a year later, in early 2004. They battled each other for domestic sales for years and now face more competition. Medtronic Inc. entered the U.S. in February, and Abbott Laboratories is headed here soon with a device -- which Boston Scientific can also sell under a profit-sharing deal -- that Wall Street analysts see as a potential market leader. Coated stents prop open heart arteries and use medication to fight renarrowing that can lead to another procedure, which is more likely with bare-metal stents. The new study included 38,917 Medicare patients who had stent procedures between October 2002 and March 2003, before any coated stent was approved, and then 28,086 patients who received stents between September and December 2003, when J&J's stent was available and was used in most stent procedures. The study found that 23% of patients treated in the bare-metal era had a repeat procedure such as angioplasty with a balloon or stent, or bypass surgery, through two years of follow-up. The rate was 19% among patients treated after J&J's stent was available. When adjusted to account for differences among patients, those treated in the coated-stent era saw an approximate 18% reduction in repeat procedures, the study said. That doesn't match the more dramatic benefit seen in randomized trails, but the fact that this study included more complex, real-world cases played a role, Dr. Malenka said. The 18% difference is "a real effect, and it's the right direction," he said. Meanwhile, the unadjusted mortality risk at two years was the same for patients in both groups, at 8.4%, while there was a slightly decreased risk of heart attacks among patients treated after coated stents were available, according to the study. The Medicare data didn't tell researchers whether patients were on anticlotting drugs. Whether patients can stick to long courses of such medication often determines today whether doctors will implant a coated stent. But a separate analysis was done to look at event rates after three months -- the time frame for anticlotting drugs with J&J's stent -- and didn't find a difference, Dr. Malenka said. |
||||
| Useful To Me Not Useful To Me | |||||
|
bengster68
Master |
25-Jun-2008 23:10
|
||||
|
x 0
x 0 Alert Admin |
Oh yes, i bird eye didn't see it clearly as it was broken into 3 lines. You are sharp, P-A-E! Is it safe to say that in DES clinical trials, they will only report "definite" and "probable" thrombosis cases? Why didn't SPIRITIII report thrombosis cases < 30 days? What duration category of thrombosis cases are the ones that causes the scare of using DES and made some doctors revert to using BMS? Some said "late thrombosis", some said "very late thrombosis", some said post 6 months thrombosis. I also understand that even BMS has thrombosis problems esp on "acute" (<1 day) and "sub-acute" (>1 but <30days) duration but not so much on "late thrombosis" and "very late thrombosis". Any comments on this area with regards to BMS thrombosis? What are the main causes of "acute" and "sub-acute" thrombosis? I have read a presntation comparing limus drugs and there was a chart stating that there are about 10 possible causes of thrombosis including durable polymer, genetic causes, etc. Some said the anti-restenosis drug that is delaying the body's natural healing progress to prevent bad scarring has help to activate an "emergency healing" and thus causes blood clots. |
||||
| Useful To Me Not Useful To Me | |||||
|
|
|||||
|
PensionAlterEgo
Member |
25-Jun-2008 22:46
|
||||
|
x 0
x 0 Alert Admin |
based on the last graph I showed for Spirit III Trial, the first pair of bar graph is for "late Thrombosis as define by ARC", which is from 30 days to 1 year. the readings is also for definite + probable. |
||||
| Useful To Me Not Useful To Me | |||||
|
allright
Senior |
25-Jun-2008 22:28
|
||||
|
x 0
x 0 Alert Admin |
Thanks trader 88. Hope you are right. Bengster and PAE, much as I admire you guys, I understand people like trader88 and cahsiertan more ha ha | ||||
| Useful To Me Not Useful To Me | |||||
|
bengster68
Master |
25-Jun-2008 22:21
|
||||
|
x 0
x 1 Alert Admin |
I have given the wrong interpretation of ARC definition of stent thrombosis on my earlier post. Under SPIRITIII RCT, the 3 cases of stent thrombosis belongs to which category (definite/probable/possible) and time (acute/sub-acute/late/very late stent thrombosis)? I think those 3 cases do not belong to "very late thrombosis" becos that SPIRITIII is for 12 months. Do they include in "possible"? Or the 3 reported cases are "definite" cases or a mix of "definite and probable" cases? P-A-E, can you help us to clarify on this stent thrombosis issue? Understanding the Late Outcomes of Drug-eluting Stents (July 2007) Much has been written, but little is known, about the long-term outcomes after drug-eluting stent (DES). The introduction of DES has extended the use of stents from a passive platform for vessel wall scaffolding to an active biotechnology vehicle for local delivery of antiproliferative pharmacotherapy. Like any other therapy or medical technology, no treatment is perfect and free of potential adverse effects or complications. Nonetheless, DES have been the most significant progress in the field of interventional cardiology, drastically reducing the rates of restenosis and need for revascularizations.1–6 Recent publications of registries and meta-analyses have raised concerns among healthcare providers and the lay public regarding the long-term safety of DES.7–13 However, these publications have been criticized as being inconclusive because of an insufficient number of patients, the absence of concurrent controls, a limited duration of follow-up, or a lack of access to original source data.14 Some common terms need to be clarified for better understanding of the subject, including the new expanded definitions of stent thrombosis, randomized clinical trials (RCTs) versus registries, on- and off-label use of stents, and the role of long-term antiplatelet therapy. To address the limitations of the trial-level meta-analyses, Stone et al. performed a patient-level pooled meta-analysis of data from nine doubleblind trials in which patients were randomly assigned to receive DES or bare-metal stents (BMS) in single, previously untreated coronary lesions through four years of follow-up. Data were used from the original databases, as defined and adjudicated by the clinical events committees for each study. Both stent types were associated with marked reductions in revascularization, an advantage that was maintained through four years of follow-up. Compared with BMS, target lesion revascularization (TLR) rates were 7.8% versus 23.6% (p<0.001) with Cyper, and 10.1% versus 20.0% (p<0.001) with Taxus. The rates of death or myocardial infarction (MI) were not significantly different between the groups with DES at any point during the four years of follow-up, and correspond to previously published natural histories of patients with coronary artery disease (CAD) treated by percutaneous coronary revascularization. Stone’s findings differ from those of some other analyses mentioned above, which suggested that overall rates of stent thrombosis and death are higher with DES than with BMS.10,11 These discrepancies may be explained by the fact that Stone et al. included only randomized double-blind studies and had full access to the complete patient-level data of the trials compared with the triallevel meta-analyses, and thus their results are more accurate. The triallevel meta-analyses relied on estimations of event rates from limited published results, abstracts, and online summaries, and therefore are not as accurate as patient-level analyses. Stent thrombosis is a dramatic clinical event associated with MI and high rates of mortality. Recent publications have suggested that DES may be associated with increased rates of late stent thrombosis and increased mortality compared with BMS. The protocols of all the RCTs with DES had a stringent definition for late stent thrombosis, demanding MI attributable to the target vessel, and angiographic documentation (sitereported or by quantitative coronary angiography) of thrombus or total occlusion of the target site, and freedom from an interim revascularization of the target vessel. It has been suggested that with this narrow definition some stent thrombosis cases may be missed, given the difficulties in defining stent thrombosis in the absence of angiographic confirmation or autopsy.4,15 Based on these principles, the Academic Research Consortium (ARC)—assembled by interventional cardiologists, investigators of DES studies, US Food and Drug Administration (FDA), and industry representatives—suggested a set of consensus definitions that will be implemented in clinical trials of DES.16 The ARC definition considers distinct reportable time-points: acute stent thrombosis (0–24 hours post-stent implantation); sub-acute stent thrombosis (>24 hours up to 30 days); late stent thrombosis (30 days to one year); and very late stent thrombosis (more than one year post-stent implantation). The ARC recognized three categories of evidence: confirmed/definite, probable, and possible. Confirmed/definite stent thrombosis was defined as the clinical event of acute coronary syndrome symptom, combined with either angiographic or pathological confirmation of stent thrombosis. Probable late stent thrombosis was defined as any MI in the territory of the implanted stent in the absence of any other obvious cause. Possible stent thrombosis included all unexplained deaths occurring at least 30 days after the procedure. It should be remembered, though, that these extended definitions are liberal and, while trying to avoid missed stent thrombosis events, they include patients who had MI or sudden death unrelated to the DES implemented years earlier. Another weakness of the ARC definitions is not excluding patients who had interim revascularization between the index DES and the qualifying event; and, indeed, probable and possible stent thrombosis were found to be more frequent after treatment for in-stent restenosis.16 Furthermore, since revascularization procedures are much more common with BMS, thromboses after interim procedures would be expected to be more common with these stents.14 With this perspective in mind the reader can understand why the overall four-year cumulative rates of stent thrombosis increased from 0.6–1.3% (protocol definition) to 3.2–3.6% (ARC definition). Whatever definition is used, the rate of stent thrombosis at long follow-up was similar, without any statistically significant differences between DES and BMS in the RCTs, 3.6% versus 3.3%, respectively, in the Cypher RCTs, and 3.2% versus 3.5%, respectively, in the Taxus RCTs.16 One single-center randomized trial needs a distinct discussion. The Basel Stent Kosten Effektivitats Trial (BASKET) Late trial extended the follow-up of the BASKET trial beyond the original six months, and evaluated the comparison of DES with BMS.9 Although there were no significant differences between BMS and DES in the rates of death and MI, a trend toward a higher rate of late stent thrombosis with DES than with BMS was noted (2.6% versus 1.3%, respectively, at 7–18 months). However, all patients with major adverse cardiac events—including death, MI, TLR, and stent thrombosis—in the first six months after stent placement were excluded from the BASKET Late analysis. This is a major flaw in the study, since the vast majority of adverse events with BMS occur in the first six months,17 thus the results are biased in favor of BMS. The major advantage of DES over BMS is in the first six months, and when combining the first six months with the following year, no significant differences between DES and BMS are noted. RCTs have the advantage of careful planning and execution with a valid control group that can lead to scientifically reliable results and conclusions. Usually, the operators in these studies are experienced interventionalists from selected high-volume centers. The study protocols adhere to relatively narrow enrolling criteria, excluding more complex clinical scenarios and anatomical conditions such as multi-vessel disease, small vessels, long segments, ostial lesions, bifurcations, bypass grafts, or restenosis lesions that are frequent in real-life interventional practice. Thus, RCTs, by enrolling relatively simple lesions in less sick patients, may underestimate adverse outcomes. Registries, despite lacking the scientifically designed control group, may report a wide range of clinical and anatomical presentations, especially if including multiple centers and a wide geographical area. On the other hand, registries should be evaluated with caution because of their frequent retrospective profile, and being aware that the data processing and adjudication of events is less comprehensive in many large-scale multicenter registries than in RCTs. Reports from outside the US presented larger patient cohorts. In a short- to intermediate-term follow-up report, including 2,229 patients from Italy and Germany treated with DES (Cypher or Taxus), the rate of stent thrombosis was 1.3%.18 The e-Cypher registry, holding more than 20,000 Cypher stent implantations in 41 countries, showed a short- and intermediate-term safety profile similar to the randomized trials, with one-year cumulative major adverse cardiac events of 5.8% and a stent thrombosis rate of 0.9%.19 Daemen et al. reported the three-year follow-up of 8,146 patients who were treated with either Cypher or Taxus stents in two large academic institutions in The Netherlands and Switzerland.20 They observed that the incidence of early stent thrombosis was similar for Cypher (1.1%) and Taxus (1.3%), but late stent thrombosis was more frequent with Taxus (1.8%) than with Cypher (1.4%; p=0.031). Late stent thrombosis occurred steadily with no evidence of diminution up to three years, at a constant rate of 0.6% per year. The largest reported registry came from Sweden, comparing 6,033 patients treated with DES and 13,738 patients treated with BMS. At three-year follow-up, DES were associated with an increased rate of death compared with BMS (adjusted relative risk of 1.18). This difference emerged after six months, when the risk of death was 0.5% higher and a composite of death or MI was 0.5–1% higher per year.13 Can the dichotomy in the outcomes of the reports with DES be explained? The answer emerges from the differences between RCTs and registries. The RCTs are the pivotal trials, providing the basic safety and efficacy data for the public health authorities (such as the FDA) to approve the use of the studied device. Based on the relatively narrow inclusion and exclusion criteria in the pivotal Sirolimus-Eluting Stent in de Novo Native Coronary Lesions (SIRIUS) and TAXUS randomized trials, the FDA has granted approval of the Cypher and Taxus stents, and labeled their use corresponding to the patients enrolled in these studies—relatively focal or short simple single lesions in native coronary arteries with diameter of 2.5–3.75mm. These represent ‘on-label’ indication. Even before the use of DES, the common use of stents included treatment of a wider spectrum of lesions such as multivessel disease, small vessels, long segments, ostial lesions, bifurcations, bypass grafts, or restenosis lesions. It has been estimated that around 60% of stent use is in such ‘off-label’ indications.21 Data from the American College of Cardiology National Cardiovascular Data Registry (ACC-NCDR) database showed that the use of DES in off-label lesions such as acute MI, in-stent restenosis, bypass grafts, and chronic total occlusions comprise 25% of all the procedures done, and were associated with low rates of short-term adverse events. In registries, usually consecutive patients are enrolled, with no, or limited exclusion criteria. Such ‘all comers’ registries represent real-world practice and include a high proportion of patients with complex disease and coronary lesions. As discussed above, registries are descriptive, and lacking a control group weakens their scientific value. In some part, RCTs and ‘real-world’ registries may complement each other and illuminate the wide range of safety and efficacy of DES. In December 2006, the Circulatory System Devices Advisory Panel of the FDA met in an effort to characterize the risks, timing, and incidence of DES thrombosis.21 The purposes of this meeting were to have a wide forum discussion on clinical data relevant to the issue of DES thrombosis and to address the appropriate duration of antiplatelet therapy after DES implantation. Based on the long-term follow-up of the randomized studies with the Cypher and Taxus stents, the panel agreed that compared with BMS, DES are not associated with an increased rate of all-cause mortality. Both approved DES are associated with a small increase in stent thrombosis compared with BMS that emerges one year post-stent implantation. However, based on the data available, this increased risk of stent thrombosis was not associated with an increased risk of death or MI compared with BMS.21 The FDA panel also addressed the broader use of DES in more complex patients and with coronary lesions—the use of a drug or device outside the FDA-approved indications. The panel stated that off-label use of DES is associated with an increased risk of stent thrombosis, death, or MI compared with on-label use. However, the panel agreed that the data on off-label use are limited, and additional studies are needed to determine optimal treatments for more complex patients. They also recommended that until more data are available, the DES labels should state that when DES are used off-label, patient outcomes may not be the same as the results observed in the clinical trials conducted to support marketing approval.21 Some parameters have been suggested as risk factors for stent thrombosis. These include stenting of complex lesions such as left main and bifurcations, chronic renal failure, prior brachytherapy, stent length, and premature discontinuation of the antiplatelet therapy.7–9,18,20,22 The latter has been clamed to be the most important risk factor, although late stent thrombosis events have been reported even in patients who were taking dual antiplatelet treatment. The occurrence of stent thrombosis in patients compliant with dual antiplatelet therapy may be related in part to antiplatelet nonresponsiveness or inadequate inhibition of platelet function.23-25 There is no wide agreement about the optimal duration of dual antiplatelet therapy to prevent stent thrombosis. Patients in the initial pivotal RCT with DES received dual antiplatelet therapy for only two to six months, but for more complex lesions, the common practice in the US—as recommended also by the American College of Cardiology/American Heart Association and adopted by the FDA panel—is to continue them for at least 12 months. In addition, since even after one year there has been pathological documentation of delayed revascularization26 and very late stent thrombosis has been reported, longer treatment may be considered for patients at low risk for bleeding, especially after long segment or complex lesion stenting. In summary, there are wide and convincing data on the long-term effectiveness of DES in significantly reducing the rates of in-stent restenosis and future revascularization. All pivotal RCTs, both individually and in patient-level meta-analysis, have demonstrated the short- and long-term safety of DES to be similar to that of BMS. However, some studies have suggested increased rates of very late stent thrombosis, especially in cases in which stents are used off-label, and with premature discontinuation of dual antiplatelet therapy. Second-generation DES are going to be approved soon, and are expected to be less prone to stent thrombosis and thus safer than the first generation DES. However, their long-term safety and efficacy will have to be proved over the coming years in post-approval studies. Late stent thrombosis will continue to be a carefully scrutinized clinical complication after DES implantation, especially in an environment where more complex lesion subsets are being treated with increased numbers of DES. |
||||
| Useful To Me Not Useful To Me | |||||
|
|
|||||
|
trader88.sg
Veteran |
25-Jun-2008 20:55
|
||||
|
x 0
x 0 Alert Admin |
OK, everyone, fundamentally Biosensors does sound good. Technically, its consolidation is coming to an end. |
||||
| Useful To Me Not Useful To Me | |||||
|
bengster68
Master |
25-Jun-2008 15:30
|
||||
|
x 0
x 0 Alert Admin |
Late stent thrombosis (as per ARC) as mentioned in SPIRITIII whereby Xience has 3 cases could be refering to post 6 months thrombosis rate. This figure could be excluding the first 6 months thrombosis cases. As for NOBORI trials, i think the stent thrombosis they are refering to includes early, late and very late thrombosis (pre-6 months and post-6 months). I remember there is absolutely zero thrombosis for up to 9 months under NOBORI 1 Phase 2 and only one non-clinically driven (out-liner) thrombosis case in NOBORI CORE up to 9 months. Comparing the TLR and thrombosis rate, looks like Biomatrix is the only DES that can beat Xience. Plus, Biomatrix's biodegradable polymer should be a good answer to late-thrombosis cases plaguing DES using durable polymer (Xience, Cypher, Taxus, Endeavor are all using durable polymer). Xience is touted to be the next DES market leader. Biomatrix should be the "next-next" DES market leader when USA FDA approval is obtained. If JNJ, MDT or BSX want to beat Abbott's Xience and become the "next-next" market leader, they need to buy BIG to achieve this goal. Xience is using BIG's older DES technology. No one else can beat Xience except using BIG's latest DES technology. |
||||
| Useful To Me Not Useful To Me | |||||
|
allright
Senior |
25-Jun-2008 15:14
|
||||
|
x 0
x 0 Alert Admin |
Its 1k sold at regular intervals of 3 minutes to .685cts. Someone has lots of time |
||||
| Useful To Me Not Useful To Me | |||||
|
|
|||||
|
allright
Senior |
25-Jun-2008 15:00
|
||||
|
x 0
x 0 Alert Admin |
Thanks PAE and Bengster. This is heavy duty stuff but so important to understand. . As to share price, someone has been selling 1k at .685 every few minutes...very irritating .. | ||||
| Useful To Me Not Useful To Me | |||||
|
PensionAlterEgo
Member |
25-Jun-2008 14:42
|
||||
|
x 0
x 0 Alert Admin |
"clinical endpoints such as TLR and MACE are typically considered more important by clinicians." as quoted in http://wwwp.medtronic.com/Newsroom/NewsReleaseDetails.do?itemId=1129556487590&lang=en_US I would also rank late thrombosis quite high as well since DES got a bad name recently because of late thrombosis. The chance of death is 40% when late thrombosis happens. Biomatrix/Nobori is currently top class in both late thrombosis and TLR readings. 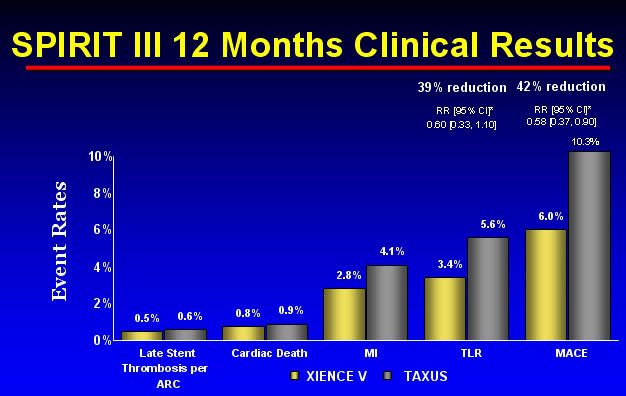
If we observe the TLR reading for Xience (Bio's closest competitor), the rates are at 3.4% (sample size = 1002). Late stent thrombosis happens in about 3 persons. 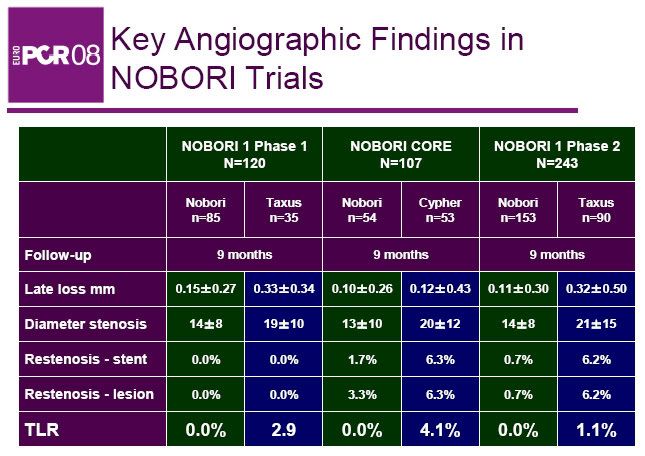
Note that TLR is ZERO for Nobori (total sample size of 470). Biomatrix has 1.3% of TLR for Stealth 1 and 0.3% for Beacon trials. Although reading above is for 9 months, 12 months reading for Nobori is still zero for TLR. AND the best thing is that Late/Very Late Thrombosis is ZERO for Nobori and Biomatrix trials so far. Remarkable so far...!!! So lets hope LEADERS keep up the same trend and we will surely see alot of buzz. |
||||
| Useful To Me Not Useful To Me | |||||
|
bengster68
Master |
25-Jun-2008 12:30
|
||||
|
x 0
x 0 Alert Admin |
Restenosis is the main reason why people use DES instead of BMS. BMS traditionally has restentosis rate of around 20%. From P-A-E's post, we can conclude that TLR is the most important very important factor to measure severe case restenosis (becos the patients need to go back hospital operating theatre and do revascularization procedures). Late-loss is used to measure how much the lesion has regrown back and is directly correlated to restenosis rate (more than 50% diameter regrown causing 75% cross-section reclogging). The higher the late-loss, the higher the chances of TLR. MACE rate is probably the most important factor as an overall guage to see how good the stent really is. It is the total number of cases of TLR, Cardiac death, Heart Attack and Heart Bypass. These are very severe cases of post stenting results and very very bad for the patients well-being (esp Cardiac Death becos it means Death!!!). TVR and TVF are not directly related to the treated lesion although but they are complications the require revascularization related to the same vessel. So i will put lesser weight on these meansurement. This is my personal ranking of importance for a DES clinical trial end-points measurement: 1. MACE rate 2. TLR rate 3. Late-loss (binary restenosis) 4. Early, Late and Very Late Stent Thrombosis rate 5. TVR, TVF |
||||
| Useful To Me Not Useful To Me | |||||
|
altius
Member |
25-Jun-2008 11:17
|
||||
|
x 0
x 0 Alert Admin |
Thank you again P-A-E and Bengster for the detailed research and information regarding this company, coronary artery disease and the PCI procedure. It is very much appreciated and extremely helpful to all of us as we struggle with our investment decisions! | ||||
| Useful To Me Not Useful To Me | |||||
|
|
|||||
|
jackjames
Elite |
25-Jun-2008 11:12
|
||||
|
x 0
x 0 Alert Admin |
oh, while we are talking here, biosensor back to 0.69 .. yeah.. oh yeah, my gf company just announced 5.2 months bonus for year 2008... that's pretty cool, next month my company will announce ours... (last year about 2.2 months only) , hopefully this year will be higher.. **praying hard**.. |
||||
| Useful To Me Not Useful To Me | |||||
|
jackjames
Elite |
25-Jun-2008 11:07
|
||||
|
x 0
x 0 Alert Admin |
yes, that is just a matter of time when we strike the 4D... ! yes! | ||||
| Useful To Me Not Useful To Me | |||||
|
bengster68
Master |
25-Jun-2008 11:04
|
||||
|
x 0
x 0 Alert Admin |
The CEO of a large DES maufacturer recently told "someone" that BIG is a very outstanding company with regards to their proprietary technology / clinical trial results and expect BIG to be a very hot takeover target. A lot of DES manufacturers license some part of their DES technology from others but what BIG has are all proprietary and BIG is still able to produce stunningly good clinical trial results. From what that CEO said, i think would-be M&A buyers of BIG are looking at BIG's proprietary IPs and clinical trial results. These 2 factors should be the biggest takeover value in BIG. CE approval and China JWMS are bonus. |
||||
| Useful To Me Not Useful To Me | |||||
|
jackjames
Elite |
25-Jun-2008 10:31
|
||||
|
x 0
x 0 Alert Admin |
Centaur..... yeah, we definitely interested in $$$$$ !! come, money come, ha ha ha... I have big patience for biosensor, no problem for that, ha ha.. maybe biosensor should become stock like this..... http://finance.google.com/finance?q=EPA:BIM maybe bengster or Pension can say some words about BioMerieux SA , any similarities between biosensor?
|
||||
| Useful To Me Not Useful To Me | |||||
|
cwwan1
Member |
25-Jun-2008 10:30
|
||||
|
x 0
x 0 Alert Admin |
Thanks p.a.e for the detail research. |
||||
| Useful To Me Not Useful To Me | |||||
|
jackjames
Elite |
25-Jun-2008 10:27
|
||||
|
x 0
x 0 Alert Admin |
ha ha.. i doubt anyone can understand the article u post, heeee... yeah, maybe you should highlight the key point, heee... summarize it mah..
|
||||
| Useful To Me Not Useful To Me | |||||
|
bengster68
Master |
25-Jun-2008 10:01
|
||||
|
x 0
x 0 Alert Admin |
I really appreciate PAE efforts to share this info with us here. PAE has probably spent a lot of time reading, researching, digesting, analysis and presenting this very detailed post. This quality of this post is of university lecturer standard! The presentation and explanation is made easy to understand for the benefit of fellow forumers. Thanks bro PAE! You are the man! | ||||
| Useful To Me Not Useful To Me | |||||
|
Centaur
Veteran |
25-Jun-2008 09:54
|
||||
|
x 0
x 0 Alert Admin |
Hi Jack, Think we won't be here if we know when is the takeover date and exact bid price lah.. Let's keep our fingers cross yah P/S: We are def interested in the $$$$.
|
||||
| Useful To Me Not Useful To Me | |||||


![[photo]](http://s.wsj.net/public/resources/images/PJ-AM639_JAMA_20080624150311.jpg)

 Ha ha..
Ha ha..